Nasal Polyps – The Current Management Process
![]()
Hi friends
We got few requests from some readers to write an article about Nasal Polyps recently, so we decided to do some research and to cover this condition in details.
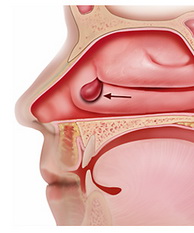
Firstly, known as the most common of the benign intranasal tumors, nasal polyps are small nasal sacs filled with fluid. These small sacs are made up of plasma cells, lymphocytes, eosinophils, and mast cells. A ciliated airway epithelium surrounds the sacs.
Around 2% of the population suffers from nasal polyps. People of all ages can present with polyps, however the chance increases with age, and peaks at 50 years. Whilst both males and females can have nasal polyps, the male to female ratio is at least 2:1. Nasal polyps is classified as a physical finding with causes and conditions, it is not classified as a disease. Approximately 25-30% of people who present with nasal polyps are asthma sufferers, and around 12% are patients with aspirin intolerance.
Nasal polyps relate to various other conditions as follows; present in 20% of cystic fibrosis patients, present in approximately 33% of patients with aspirin intolerance, present in 2% of chronic rhinosinusitis patients, present in 7% of asthma sufferers, present in 50% of Churg Strauss Syndrome (the eosinophilic vasculitis), present in most patients with allergic fungal sinusitis, present in various ciliary motility disorders such as Kartagener’s Syndrome, present in various genetic syndromes like Young’s Syndrome, present in 0.1% of children. When nasal polyps are seen in a child under 16 years of age, evaluation should include a sweat chloride test.
As previously noted, nasal polyps shows a direct relation to asthma and aspirin intolerance. When these three factors show together, they are known as the aspirin triad, or Samter’s Syndrome. It is estimated to be prevalent in 20% of severe asthma patients, and 2-3% of general asthma patients. Typical patients show the following conditions; middle-aged, white, shows vasomotor rhinitis, has perennial bronchial asthma, eosinophilia, presents negative skin tests to atopic allergens, aspirin (and other related chemicals) intolerant. In general, the reaction starts from 15 to 180 minutes following ingestion. The reaction is characterized by severe rhinorrhea, macular erythema, nausea, vomiting, diarrhea, and cramps in the intestines. These symptoms are followed by an acute bronchial asthma attack. Recovery time for most patients is 2 hours.
Although the above facts are known, the specific etiology of polyps is still currently unknown. Possible mechanisms contributing to the development of nasal polyps include the following: infection, allergy, mucopolysaccharide abnormality, sensitivity to a certain drug, autonomic imbalance, enzyme abnormality, histamine, proto-oncogene and mechanical obstruction. It appears that allergy and infection are currently viewed as the most likely causes.
Most patients firstly complain of nasal obstruction, many also mention allergic complaints such as sneezing, watery rhinorrhea and itchy eyes. Headache, postnasal drip and asthma are also commonly noted. When asked, others mention insomnia as a symptom. Acute infections present pain in the patient. Some patients have middle ear pathology, or have developed rhinitis medicamentose from the use of chronic vasoconstrictor. A high percentage of patients have previously had nasal surgery.
Despite being the most common of the benign intranasal tumors, diagnosis can include meningoceles or meningomyeloceles, possibly projecting through the nose by means of a dermoid cyst or a cribriform plate defect. Tumors such as squamous cell carcinomas and inverted papillomas can also show symptoms similar to nasal polyps. Neoplasms, however, are generally firm and bleeding tends to be spontaneous.
When it comes to treating nasal polyps, medical or surgical management is used, at times treatment requires a combination of them both. Eliminating the polyps and rhinitis symptoms, is the ultimate goal of treatment. Treatment also aims to restore nasal breathing and olfaction, and to provide a preventive measure, without the unneeded removal of sinus pathology. Since many patients are free of symptoms, even though their CT scan shows sinus opacification, complete removal of sinus pathology does not appear to be a realistic treatment plan.
Where a patient complains of a disruption to their quality of life, surgery is considered as a treatment option, particularly for patients who have not seen results from substantial medical therapy, or patients with a contraindication to an area of medical therapy. Since surgery is elective, many understand it to be a feature of a continuum of therapy, rather than independent of medical treatment. It should be noted that surgical removal of nasal polyps does not always prove to be the solution. Where a patient also presents with asthma, the decision of surgery should be carefully considered, often with a need to increase steroid doses if the decision goes ahead.
The follow-up of patients who underwent endoscopic sinus surgery for nasal polyps, has been documented in several series. Such studies have varied from 100 patients to as many as 250, follow-up has varied from 18 months to 4 years after surgery. Treatment outcome is generally assessed by analyzing the patient satisfaction, based on relief of symptoms. Assessment also takes into account an examination of the sinonasal area. Where follow-up was between 1-4 years, 80-90% of patients showed a symptom improvement, however this percentage drops when considering patients who are completely symptom free. Objective evidence has also presented, in patients with an improvement in nasality of speech and an unilateral reduction of airflow resistance.
Reviewing 120 patients who underwent endoscopic sinus surgery, Kennedy reports that 28% had diffuse polyposis and 31% suffered from polyps which arose from the middle meatus. His findings showed that the preoperative level of the disease, was the key predictor of symptom improvement. Underlying conditions, such as Samter’s triad or asthma, may have an influence on the severity. The finding that such patients have a tendency to fare worse, has been noted by other researchers. Patients who are surgical patients, and suffer from nasal polyps, often have a much more complex disease involvement.
Taking all factors into consideration, it could be said that certainly nasal polyps are the most common benign intranasal tumor. Whilst their specific etiology is not known, there is an association with other diseases. A continuum of medicine and surgery are seen to be the general treatment path, however surgery is recommended only in patients who present with a severe condition or have failed to see results from substantial medical therapy. Treatment focuses on controlling the condition.
Disclaimer: This information is from documents that were prepared by resident physicians for presentation and discussion at a conference held at Baylor College of Medicine in Houston, Texas. This material should not be used as a basis for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed medical literature.

 Hey everyone and thanks for stopping by! We hope that you will find our detailed reviews to be useful for you. Feel free to get in touch if you have any question... All the best! Rita and Alex
Hey everyone and thanks for stopping by! We hope that you will find our detailed reviews to be useful for you. Feel free to get in touch if you have any question... All the best! Rita and Alex 